Healthcare Denial Management
The client is a large multinational provider engagement company that provides healthcare solutions. It wanted to build a solution that will reduce the costs associated with the preliminary vetting of claim files; highly complex 837 & 835 EDI files and healthcare claim processing. Several historical features were engineered to capture the context of the whole denial management process. Leveraged a machine learning model and a complex neural network model to predict the denial status, denial reasons, and paid amount by the insurance provider of healthcare claims.
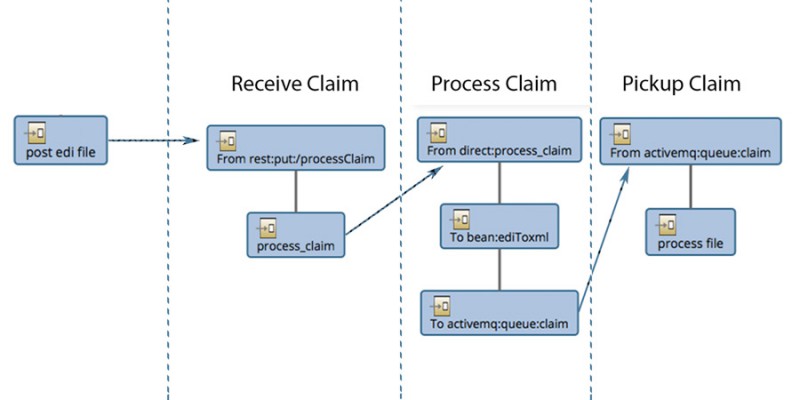
The whole end-to-end process was packaged into a single API which reduced the substantial manual work in the claim management process.